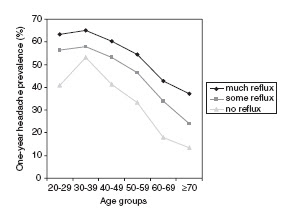
 A large study conducted in Norway points at some definite links between headaches and GI tract complaints like acid reflux (see figure on the left), nausea, constipation, and diarrhea. Over 60,000 people participated, and the results were adjusted for sex, age, education, depression, anxiety and use of medication. The clearest connection was between headache frequency and GI symptoms (rather than severity, or simple headache occurrence). All reported symptoms were evaluated clinically (quite a feat!) and so there is some measure of objectivity to the data as well.
A large study conducted in Norway points at some definite links between headaches and GI tract complaints like acid reflux (see figure on the left), nausea, constipation, and diarrhea. Over 60,000 people participated, and the results were adjusted for sex, age, education, depression, anxiety and use of medication. The clearest connection was between headache frequency and GI symptoms (rather than severity, or simple headache occurrence). All reported symptoms were evaluated clinically (quite a feat!) and so there is some measure of objectivity to the data as well.The authors rightly point out that, while there's been a decent smattering of research on migraines and GI complaints (esp. nausea), none has been conducted on headaches in general. This is interesting because to me a non-migraine headache is more indicative of generalized neuromuscular tension and inflammation, and thus we might speculate that this study shows that GI tract irritation is linked to inflammation in other parts of the body. Which came first is not as important to me as the fact that an intervention in the gut may be able to help inflammation in areas far from the gut. In the author's words,
"There is anatomical and functional evidence of convergence between nociceptive and viscerosensory systems involved in reflexes and homeostatic and behavioural control of autonomic outflow".Now of course, this is not news to herbalists. Demulcent herbs (like Flax) have long been used to alleviate not only GI tract inflammation (most directly), but also respiratory, urinary tract, and neuromuscular inflammation. Simon Mills' concept of acupharmacology (an excellent overview on page 11 of this newsletter) does a lot to explain these mechanisms in more detail. But I am heartened to see this trend in modern medicine (see the now mainstream asthma/reflux connection): perhaps there are linkages between different functional processes in the physiology... perhaps dietary influences on the GI tract can actually help issues elsewhere... maybe human beings need a more broad approach, one that encompasses their bellies, their spirits, and their individual constitutions. Or, at least, as the authors conclude:
"It is important to consider the total burden of discomfort in these patients in order to provide for the best treatment, and the prognosis as to overall function may be determined not only by headache, but also by the comorbid conditions".So careful with high-dose NSAIDs for those chronic headaches - it might upset an already upset belly. Well, at least it's a start...